新しいAGA治療薬ザガーロは通販でどこが安い?

新しいAGA治療薬として販売された「ザガーロ」を安く購入するには、海外通販がオススメです。
そもそもザガーロは、前立腺肥大症の薬「アボダート」として、世界102カ国以上で承認された医薬品です。
日本では「アボルブ」という名称で、前立腺肥大症の薬として承認されていたのですが、発毛効果が認められてからは、日本では新たにAGA治療薬「ザガーロ」として発売されました。
有効成分はどれも同じ「デュタステリド」なので、「ザガーロ」「アボダート」「アボルブ」は、名前違いますが同じ医薬品となるのです。
ザガーロはどこで買えるの?
ザガーロは、クリニックで処方してもらうか、海外通販で購入します。
クリニックと通販ではどう違うのでしょうか?
そこでクリニックと通販の違いについてまとめてみました。
| クリニック | 通販 | |
|---|---|---|
| 初診料 | 2,000円 | なし |
| 再診料 | 1,500円 | なし |
| 送料 | なし | 1,000円 |
| 薬代 1ヵ月分 |
9,000円 | 4,500円 |
| 1回利用分合計 | 11,000円 | 5,500円 |
表のように通販ならクリニックの半分の値段で購入できます。
それでは詳しく見てみましょう。
通販とクリニックの違い
安く購入するには通販の方がいいのですが、ほかにはどういった違いがあるのかご説明します。
| クリニック | 通販 | |
|---|---|---|
| メリット | ・正規品を扱っている ・状態を確認してもらえる ・アドバイスがもらえる |
・値段が安い ・誰にもバレない ・家にいながら買える ・手続きが簡単 |
| デメリット | ・値段が高い ・買いに行かなければならない ・身内にバレる |
・届くまで時間がかかる ・悪質なサイトもある |
クリニックに向いている人
クリニックの場合、診察をしてから薬を処方してくれるので、現状の自分を確認できます。
そして、どのように対処していけばいいのかアドバイスをもらえるので、どうしたらいいのか悩んでいる人はクリニックに相談した方がいいでしょう。
また、薬は医師が処方する正規品がいいと考えている人は、クリニックなら正規品を処方してもらえるので安心できると思います。
ただ、AGA治療は保険適用外の自由診療になるので値段が高くなります。
その他、診察料がかかる、時間を合わせてクリニックに通わなければならない、家族にバレるなどあります。
そのため、クリニックに向いている人は
- 自分の現状を知りたい
- アドバイスが欲しい
- 正規品を使用したい
- 時間の融通が利く
- 家族などに知られても大丈夫
上記にあてはまる人なので、自分と照らし合わせてみて下さい。
通販に向いている人
クリニック以外では、海外から通販で購入できます。
通販なら、診察料や処方箋なしでクリニックよりも安く購入できます。
また、忙しい人でもネットが繋がる場所ならどこでも購入できるのです。
ただ、海外から発送されるので、届くまで時間がかかってしまいます。
- 安く買いたい
- 誰にもバレたくない
- クリニックに行く時間がない
- 手軽に買いたい
手軽に買いたい、安く買いたいといった人や、忙しくてクリニックに行く時間がない人にも向いています。
通販できるザガーロ
日本でAGA治療薬として承認されているザガーロは通販で購入できません。
しかし、ザガーロと同じ有効成分デュタステリドが配合されているAGA治療薬は、通販できる商品もあります。
アボダート
グラクソ・スミスクライン社が販売している前立腺肥大症の治療薬で、なんと世界102カ国以上で承認されています。
男性ホルモンのテストステロンに作用し、病気の原因となるジヒドロテストステロンに変換するのを抑制します。
この作用はAGA治療と同じで、ジヒドロテストステロンに変換するのを抑制して抜け毛を防ぐのです。
| サイト名 | ネットの くすり屋さん |
薬の通販 オンライン |
あんしん 通販マート |
お薬通販部 |
|---|---|---|---|---|
 |
 |
 |
 |
|
| 1ヵ月分 | 4,500円 | 5,980円 | 6,480円 | 4,519円 |
| 2ヵ月分 | 8,100円 | 10,764円 | 11,794円 | 9,160円 |
| 3ヵ月分 | 10,800円 | 15,608円 | 16,913円 | 13,010円 |
| 1錠最安値 | 120円 | 161円 | 179円 | 144円 |
一番安く販売しているのは、ネットのくすり屋さんでした。
また、どのサイトも複数購入すると、1箱当たりの値段が安くなっています。
安くザガーロを通販するならジェネリックがオススメ
ザガーロは通販で購入した方が安いと説明してきましたが、その中でもジェネリック医薬品を選んだ方がお得に購入できます。
まずクリニック、ザガーロ、ジェネリックの値段を比べてみましょう。
| クリニック | 通販 ザガーロ |
通販 ジェネリック |
|
|---|---|---|---|
| 1ヵ月 | 9,000円 | 4,500円 | 2,700円円 |
| 1錠あたり | 300円 | 150円 | 90円 |
ザガーロは通販ならクリニックの半分ほどで購入できますが、ジェネリックならさらにその半分ほどの価格で手に入れられます。 ではザガーロジェネリックはどのようなものがあるのでしょうか?
オススメのザガーロジェネリック
通販を利用するにも安くデュタステリドの薬を購入するなら、ジェネリック医薬品が安くてお得です。
そもそもなぜザガーロジェネリックが安いのかと言うと、グラクソ・スミスクライン社ではない会社が同じ有効成分を使って作った医薬品で、開発費や研究費がかかっていないからです。
そんなお得なザガーロジェネリックは複数存在します。
ではどのザガーロジェネリックがいいの?と思いますよね?そこで、ここではオススメのザガーロジェネリックを紹介いたします。
| 商品名 | デュタストロン | デュプロスト | デュタス |
|---|---|---|---|
 |
 |
 |
|
| 値段 | 30錠 2,700円 | 100錠 9,000円 | 30錠 3,150円 |
| 1錠あたり | 90円 | 90円 | 105円 |
| 特徴 | コスパが良い | 100錠から販売 | 人気がある |
| 詳細はコチラ | 詳細はコチラ | 詳細はコチラ |
デュタストロン

インドのレクメズ社が開発したAGA治療薬で、開発に日本人が関わっていたので日本人向けの作用となっています。
副作用も感じにくく、続けやすいオススメのAGA治療薬です。
| サイト名 | ネットの くすり屋さん |
薬の通販 オンライン |
あんしん 通販マート |
お薬通販部 |
|---|---|---|---|---|
 |
 |
 |
 |
|
| 1ヵ月分 | 2,700円 | なし | なし | 2,800円 |
| 2ヵ月分 | 5,100円 | なし | なし | 5,320円 |
| 3ヵ月分 | 7,200円 | なし | なし | 7,560 |
| 1錠最安値 | 70円 | なし | なし | 93円 |
| なし | なし |
デュタストロンはとても安くてお得で、ネットのくすり屋さんが最安値です。
デュプロスト

シプラ社が開発したAGA治療薬で、100錠単位で販売しているので、多く購入したいと考えている人に向いています。
ネットのくすり屋さんなら、最安値で購入できます。
| サイト名 | ネットの くすり屋さん |
薬の通販 オンライン |
あんしん 通販マート |
お薬通販部 |
|---|---|---|---|---|
 |
 |
 |
 |
|
| 100錠 | 9,000円 | 9,980円 | 9,980円 | 8,290円 |
| 200錠 | 16,200円 | 15,968円 | なし | 15,750円 |
| 300錠 | 21,600円 | なし | なし | 22,380円 |
| 1錠最安値 | 72円 | 80円 | 100円 | 74円 |
デュタス
ドクターレディー社が製造販売しているザガーロジェネリックです。
最近人気が上がっているザガーロジェネリックで、効果は先発薬と同等で値段は安くなっています。
| サイト名 | ネットの くすり屋さん |
薬の通販 オンライン |
あんしん 通販マート |
お薬通販部 |
|---|---|---|---|---|
 |
 |
 |
 |
|
| 1ヵ月分 | 3,150円 | 4,880円 | 4,880円 | 2,950円 |
| 2ヵ月分 | なし | 7,808円 | 8,101円 | なし |
| 3ヵ月分 | 8,500円 | 10,980円 | 11,126円 | 8,410円 |
| 1錠最安値 | 84円 | 107円 | 109円 | 88円 |
デュタスはお薬通販部が最安値ですね。
AGAコスパ最強セット
デュタステリドは、抜け毛を防いで頭髪を増やしていきますが、同じAGA治療薬の「ミノキシジル」は直接毛根に働きかけて、髪を発毛、育毛する作用があります。
この二つを併せて使えば、デュタステリドで抜け毛を防ぎつつ、ミノキシジルで力強く育毛できます。
どれを買えばいいのか悩んだ人は取り敢えずこのセットがオススメです。

| 3ヵ月 | 6ヵ月 | |
|---|---|---|
| 錠数 | 180錠 | 360錠 |
| 値段 | 9,000円 | 16,000円 |
| 販売サイト |
6ヵ月分がかなりお得になってるので、続けるなら6ヵ月分がオススメです。
ザガーロとプロぺシアとの違い

世界初のAGA治療薬であるプロペシア。
ザガーロはプロペシアよりも優れた作用を持っています。
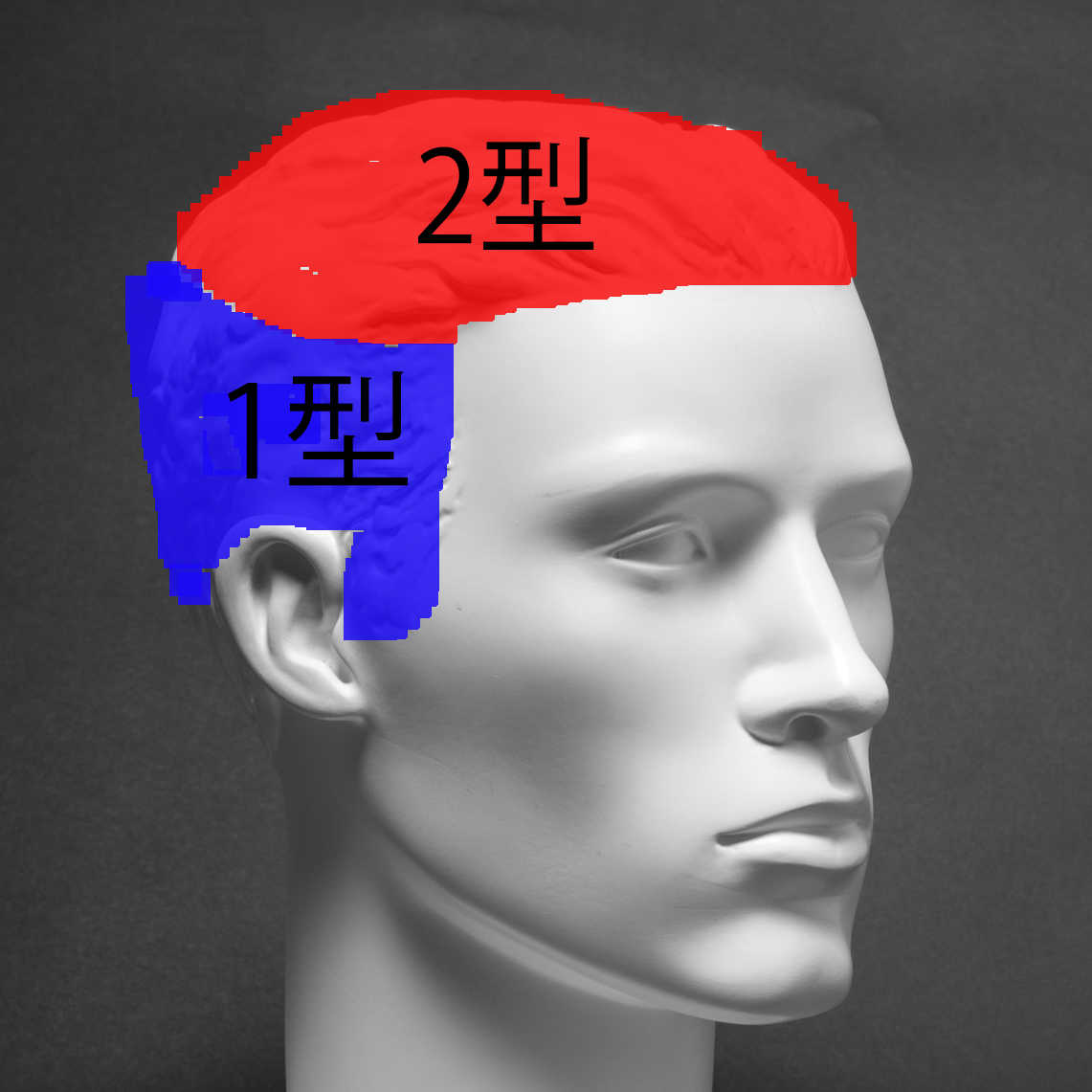
AGAの原因は5αリダクターゼⅠ型とⅡ型という2つの原因物質から起こります。
プロペシアはこのうちⅡ型に作用をし、抜け毛を防ぎますが、Ⅰ型には作用しません。
しかし、ザガーロはこのⅠ型とⅡ型の両方に作用して抜け毛を防ぐのです。
 |
|
|---|---|
| Ⅰ型 | 側頭部、後頭部 |
| Ⅱ型 | 前頭部、頭頂部 |
ザガーロを通販するメリット

ザガーロの通販は海外から個人輸入をするのですが、どういう仕組みなのかメリットやデメリットなど詳しくご説明いたします。
安く購入できる
海外医薬品の通販の項でも書きましたが、通販なら診察料や初診料などかかりません。
クリニックではザガーロが処方されますが、値段も高額になっています。
通販では、同じ有効成分のデュタステリドを使用しているアボダートが安く購入できるし、もっと安いジェネリック医薬品も選べます。
誰にもバレない
AGA治療をおこなう時に、家族や友人には知られたくないと考えている人もいるでしょう。
クリニックだと空いている時間に行くので家の人には怪しまれ、クリニックの前で知り合いとすれ違うなんてこともあるかもしれません。
通販なら、家や郵便局で受け取れるし、中身がなにかわからないようになっているので、誰にも知られずにAGA治療がおこなえるのです。
ネットが繋がる場所ならどこでも購入できる
海外通販は、amazonや楽天のように、普通のネット通販と同じような感覚で購入できます。
スマホがあれば、どこからでも手軽に注文できるんです。
仕事が忙しくてクリニックに行く時間が取れない、家族サービスもあってなかなか自分の時間が作れない人にピッタリです。
海ザガーロを通販するデメリット

安くてお得な通販ですが、デメリットもいくつかあります。
利用する前に確認して、失敗しないようにしましょう。
商品が届くまで時間がかかる
医薬品は海外から発送されるので、14日~1ヵ月ほどかかる場合があります。
購入しようと考えている人は、早めに購入しましょう。
AGA治療は、6ヵ月ほど続けることになるので、1月分を切る前に次の分を購入しましょう。
ニセモノの可能性がある
残念ながら悪質なサイトもあって、偽物が送られて来ることや、医薬品が届かないこともあります。
悪質なサイトにだまされないために、優良なサイトの条件をご紹介します。
- 継続年数が長い
- 責任者や所在地が明記されている
- 電話で問い合わせができる
- メールなどの問い合わせが丁寧で早い
- 値段が安すぎない
これらのポイントを確認して、優良なサイトを選びましょう。
ザガーロを通販で購入する方法

海外通販(個人輸入)の手順
海外通販は普通のネット通販と同じで、商品を検索し、数を指定して、名前や住所を記入して、お金を払うだけです。
詳しくは下記のページで確認してみて下さい。
Amazonや楽天では購入できない
デュタステリドを通販で買おうとした人は、Amazonや楽天で出てこなくて驚いた人もいるでしょう。
デュタステリドは、医師の処方箋がないと購入できないので、Amazonや楽天といった通販では購入できないのです。
ネットでデュタステリドを購入するには、処方箋が必要ない海外通販を利用するしかありません。
ザガーロを使った人達の口コミのご紹介

ここで実際に使用した人の感想を確認してみましょう。
引用:https://www.bestkenko.com/products/%E3%82%A2%E3%83%9C%E3%83%80%E3%83%BC%E3%83%88#tabsコスパ最高!
ザガーロを病院で貰うと一ヶ月分で10,500円もするのに、この商品の値段なら長く続けられそうです。
ザガーロを飲んで3ケ月、この薬を飲み始めて1ヶ月なのですが、まだ実感はあまり感じられません。
6ヶ月後を期待して飲み続けてみたいと思います。
引用:https://okusurinavi.shop/prd_review.php?pid=610#item_reviewもう使用して、1年くらいになります。効果ありますよ。 それまでクリニックに通って今いたが、ドクターが血圧はかって薬を出すだけでの10分診療で、1か月分で16000円も取るので、高くてアホくさくて自分で買うことにしてネットでこの薬をみつけました。 ちなみに、そのドクターが処方してくれたのは、1日あたり、 デュタステリド 0.5mgx2錠ミノキシジル 5mg x 1錠 でした。 が、念のため私は現在、各1錠で運用していますが、現状維持以上には効果があります。 恐らくオーダーしてから輸入なので、到着までに2-4週間くらいかかりますが、スケジュールでオーダーしておけば問題ありません。 もちろん、私の場合は副作用など一切ありません。 小粒で飲みやすいですし。 これから続けます。
引用:https://www.unidru.com/products/avodart#tabsこちら使い始めてから半年経ちましたが、目に見える程増えました。
周りからもどうしたの?と言われる程です。
もうやめられません。
通販ならザガーロを続けやすい理由

通販なら、ネットが唾がる環境ならどこからでも安く購入できます。
それに誰にもバレずに購入できるので、気づいたらフサフサになってて、みんながビックリするでしょう。
AGA治療をするなら、デュタステリドを通販で続けるのがオススメです。

 購入する
購入する 購入する
購入する 購入する
購入する 購入する
購入する